Minimally
invasive diagnostic procedures in patients with inflammatory breast cancer and
negative imaging test
Authors: Saribekyan E.K., Stepanov
S.O., Guts O.V.
PA Hertsen Moscow Oncological Research Institute,
Russian Federation
ABSTRACT
We have studied peculiarities
and problems in order to determine whether or not cancer is present in
“diffuse” forms of a breast cancer cases (IBC, for example) when breast imaging
techniques usually have not found breast cancer. The most effective technique
that takes a sample for cancer verification is US –guided core needle biopsy.
We prefer take tissue samples from the most suspicious areas of a breast with
indirect tumor sights and also taking samples from areas of a breast where the
breast cancer detected very often – in upper lateral and central areas of a
breast. Vacuum-assisted breast biopsy has many advantages in comparison with
traditional core needle biopsy and fine-needle aspiration in order to get
reliable result when imaging is not clear.
Key words: “diffuse” breast
cancer, minimally invasive diagnostic,
breast biopsy
Correspondence to: Erik
Karlovich. E-mail: mammolog3@yandex.ru
Introduction.
The breast cancer takes the first place among malignant tumors at women. Diffuse
form of breast cancer (such as IBC) accounts for 15-17% of all
breast cancer cases [4].
Diffuse form of breast cancer is
characterized as enlargement one of the breast combining with thickening of the skin and
redness. Inflammatory breast cancer is
an edematous affection with skin changes like an orange peel and nonpalpable
lesion with diffuse structure, fast growing tumor
mass. IBC grows and spreads so quickly and it is
harder to treat successfully this type of breast cancer [1, 7]. The most common symptom in patients with IBC is nonpalpable lesion
without clear boundaries.
IBC is an especially aggressive form of breast
cancer. The features of clinical
manifestation of “diffuse” breast cancer with mastitis symptoms can lead to
diagnostic errors and delay to initiation of treatment.
The last decade
has witnessed the rapid development of imaging techniques and methodologies
in cancer diagnostic. There are ultrasound,
digital x-ray mammography, CT, MRI, biopsy under
X-ray or ultrasound
guidance [2,6]. Modern diagnostic
equipment allows us to detect breast cancer 4mm diameter
or less, and take the cells for cancer verification using
fine-needle biopsy. In this case, each method has the features and limitations,
depending on the physical properties of breast
tissue and the nature of cancer [3,
9].
X-ray mammography is
more informative in women older than 40 years with the prevalence
of involutive processes in the breast glands and fatty tissue. Marked glandular
component and the hyperplastic tissue more
typical for young women, and these peculiarities
reduced the possibility of X-ray visualization of structures
that are "lost" in the hyperplastic
tissue array. In
this situation ultrasound becomes more informative.
CT scan (compared
with ultrasound and mammography)
shows the tumor more
precisely located in retromammarnuyu
space and the extent of tumor on
the chest wall that is important in the
planning of surgical intervention and treatment. CT clearly
diagnosed thickening of the structural
pattern of the breast, skin thickening in cases of IBC, increasing the size of one breast. However
the restructuring of the
surrounding tissue and tumor
hypervascularity in breast more
accurately visualized with
mammography [10]. The method of
MRI has high sensitivity (100%) and specificity (90%). MRI
performed in the tomograph
with the magnetic field intensity of
1.0 T. The study
was conducted before and after
intravenous administration of contrast agent [8].
The patient is placed on
the abdomen and breasts are placed in special mammographic "coil"
which create the necessary compression. The diagnosis of cancer put upon
detection of nodules, if the lesion is intensely and diffusely increased during
the first two minutes after administration of contrast agents. Information
about using MRI in diagnostic of IBC and other diffuse forms of breast cancer
in the world literature is insufficient for the specific recommendations [5, 11]. In addition, using of MRI is limited by high cost,
complexity and duration of the study, the presence of “coils” only for the same size breasts.
Performing a biopsy under MRI – guidance has become possible in recent years;
however it is technically more difficult manipulation compared with biopsy
under X-ray or US– guidance.
Thus, “diffuse” forms of cancer without
clear boundaries of the tumor especially in combination with fibrous tissue may
be difficult in diagnosis despite using modern imaging techniques. It extends
the period of investigation and delayed the start of appropriate treatment.
Increasing the number of outpatient visits the patient also contributes to high
financial costs of medical institutions.
Materials and methods.
Studied
the results of the survey in 26 patients in whom the presence of direct and indirect symptoms of breast
cancer did not allow to visualize and verify the tumor during
the preliminary examination. The
study was conducted in Hertsen
Moscow Oncological Research Institute for the period 2007- 2010.
All patients had a clinical picture of IBC. They complained of enlargement
and protrusion of the quadrants or the entire breast, pain
and discomfort in the breast, feeling
the bloating in the breast. Most of the patients (20 women) were examined in connection with suspected infiltrative-edematous symptoms such as swelling,
skin changes like an orange peel combined
with warmth and edema . In 8 patients we identified and verified metastases in the axillary lymph nodes. Immunophenotyping
showed that metastasis spread from breast cancer (three of patients –
without detected lesions in the breast
after total medical inspection). 6 patients submitted to Hertsen Moscow Oncological
Research Institute after due to presence suspicious sites identified after medical examination (palpation,
mammography and ultrasound). Age of patients ranged from 30 to 72 years (mean
age was 51.4 years).
All the patients before treatment
in Oncological Research Institute and during
the initial survey were made mammography and ultrasound.
In addition, CT scans performed in 7 patients, MRI – in 4 patients. All patients were attempts to verify the diagnosis. We took
samples of tissue for morphological studies in the areas
where presumably could localize the tumor. We used well known biopsy
techniques: fine needle aspiration
biopsy with / without US- guidance (26 patients), vacuum− assisted biopsy under X-ray guidance (3), open surgical biopsy
of the skin in the areas of swelling of the skin (4), sectoral resection (3). The number of biopsies in
the manipulation of a single
method was from 1 to 3, repeated
biopsies were performed only after fine-needle biopsies in 12 people.
In connection
with the problem of verification of the
diagnosis, all patients are directed to the study of minimally invasive procedures, which performed
the final diagnostic procedure.
Equipment of examination room includes a
vacuum biopsy device "Mammothom", equipped with paddle
handles with needle
gauge 11G and 14G in the assembly "Endo-Surgery Etikon, Inc.", corporation "Johnson and Johnson"
(USA, Mexico), spring loaded biopsy systems
BARD, ultrasound scanners SONOLINE with Siemens Medical Solution accessories
(USA).
To obtain
tissue samples for histological examination we made biopsy in
areas with indirect signs of tumor under US - guidance, and arbitrarily
in places the most frequent localization of IBC -
in the upper outer and central
quadrants. The choice of needle gauge for biopsy
(from 14 to 11G) was determined according to the size of the breast, expression changes in the breast and the physical density of the breast tissue. Samples
of the breast tissue after biopsies was labeled,
numbered and reflected in the scheme
which was annexed to the direction of
the histological examination. This
technique called multipoint
arbitrary and automatic vacuum -biopsy under
US- navigation.
We
considered as a possible presence of indirect signs
of tumor areas with
hyperechogenicity, abnormal vascularity in the Doppler, the concentration of tubular structures, US and clinical (inspection, palpation) picture of the differences with the healthy breast. We paid special attention to areas with severe fibrosis. Our experience has shown
that the application of medical imaging techniques mostly
do not notice tumor located below the
array of fibrous tissue.
Selection of the
most frequent localization
is based on a study carried out in Hertsen Moscow
Oncological Research Institute. We studied the
frequency of tumor in IBC
cases, composing the
vast majority in the structure of the “diffuse” form of
breast cancer. In 288 patients
we examined the localization of the breast tumor in breast quadrants, quadrants borders and central areas. The most frequent localization was the upper-outer quadrant - 29,5% ± 2,7, central areas - 17,0%± 2,2.
Case report.
Patient ZH.N.S., 71 years,
Diagnosis: Cancer
of left breast cancer stage IIB, T2N1M0.
From the history:
In July 2010 patient found changes in the left breast as a protrusion in the
upper areas of the breast. She was examined in Hertsen Moscow Oncological Research Institute As a
result of a comprehensive examination (medical
inspection, palpation, ultrasound, mammography) we
obtained fibrosis. Mammography report (17.08.10): in the left
breast the border of the upper
quadrant is marked
with a restructuring of the seal in the center of the
fibrosis type. The right breast is
without focal pathology.
However despite the mammography and US results, the clinical did not allow rejecting diagnosis of the breast cancer.


Picture1. Inspection of the breasts.
Swelling in upper
and central quadrants of the left breast.
Hematoma after
fine-needle biopsy.
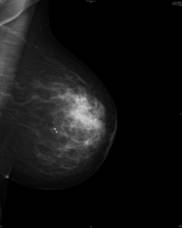
Picture 2. Mammography Picture
3. Mammography
of the left breast. of the right breast .
Fibrosis structure. Without focal
pathology .
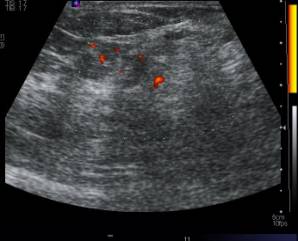
Picture 4. US
picture with Doppler of the left breast.
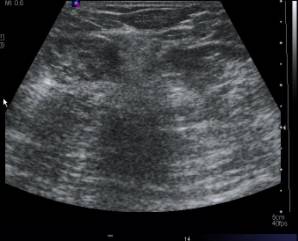
Picture 5. US
picture of the left breast.
The patient was redirected
to ultrasound examination into for microinvasive multipoint vacuum-biopsy
under US-guidance. After histological examination was diagnosed lobular carcinoma. 30/08/10
surgical operation: radical mastectomy
on the left. Histological conclusion ¹ T 48729-47/op
on 06.09.10:
tumor in the central parts of the site without
clear boundaries sizes 3.5Õ2.5õ3
cm. Iinfiltrative lobular carcinoma
grade 2 (7
points) with the presence of
tumor embolls in the lumen of
lymphatic vessels. 4 lymph nodes - lobular cancer
metastasis without invasion
beyond the capsule. Postoperatively,
radiation therapy is carried out and courses of chemotherapy according to the scheme CAF. At follow-up
examination one year after the operation - with no signs of
recurrence.
The results of treatment.
Histological examination of material obtained by multipoint arbitrary
vacuum-biopsy under US-guidance in all these cases established
to define diagnosis. In two cases, after an
automatic biopsy performed
with uninformative material we made vacuum-biopsy. Repeated manipulation after
vacuum-biopsy did not needed. In
22 cases (84.6%) was verified
breast cancer, in 2 patients
was diagnosed fibrosis of the tissue,
in 1 patient - chronic mastitis. In one patient
the bright clinical picture of IBC (edema
and redness of the skin of breast)
was due to thrombosis of the veins extending from the subclavian vein. All
cases of non-malignant changes
were confirmed by the observation
periods of 6 months and more. Histological forms of breast cancer: ductal cancer– 10 cases, lobular cancer – 5 cases, the combined ductal and lobular – 6 cases, intraductal
cancer – 1case. The
results of the various minimally
invasive diagnostic methods
are presented in Table 1.
|
Types
of biopsies |
Number
of biopsies |
Number
of repeated
biopsies |
Cancer
verification |
Average
number of tissue samples due to usual biopsy |
|
Automatic
biopsy |
10 |
2 |
9 (90%) |
5 |
|
Vacuum-biopsy |
16 |
- |
16 (100%) |
4 |
Table 1.
Conclusion:
Due to examination of patients with diffuse form of breast cancer by medical
imaging may be significant errors in diagnosis and complexity of cancer verification in cases
with undetected tumor, despite the high spreading the process. The
most difficult for diagnosis are cases of tumor in located in or under an array of severe fibrous
tissue.
In cases of getting uninformative
material after fine-needle biopsy the most effective method of obtaining tissue samples for verification is multipoint vacuum-biopsy of suspicious areas and biopsy sites the most frequent localization of “diffuse” cancer
- in the upper-outer and central quadrants in the breast. Vacuum-assisted breast biopsy has many advantages in comparison with
traditional core needle biopsy and fine-needle aspiration in order to get
reliable result when imaging is not clear. But the
final choice made by the specialist
individually.
Manipulation should be performed highly skilled and experienced professional.
References.
1. Pak D.D., Saribekyan E.K. / Chapter
"Tumors of the breast" in Russian Oncology Guide. Ed. V.I.Chissova,
S.L.Daryalovoy. -M. LLC "Medical News
Agency," 2008. - p.382-408.
2. N.V.Ponedelnikova, G.P.Korzhenkova, V.P.Letyagin, Ya.V.Vishnevskaya. Selecting the method of verification of
palpable space-occupying lesions of the breast at the preoperative
stage. Tumors of the female
reproductive system. -2011 - N1- p.41-45.
3. Guidance in Radiodiagnostic
techniques in evaluation of breast disease,
edited by prof. G.E. Trufanova - "ELBI-Petersburg" - St. Petersburg. - 2009. - p. 192-281.
4. Condition of cancer care in
Russia in 2009. Edited by V.I. Chissov, V.V.
Starinskiy, G.V. Petrova. Moscow,
2010.
5. Fisher W., Baum, F., Lyuftner-Nagel C./Chapter “Medical Imaging”, Diseases of the breast, edited by B.I.Dolgushina. M. MEDpress-Inform, 2009. p.10-190.
6. V.P. Harchenko, N.I. Rozhkova/Chapter “Edema syndrome
of the breast”, Radiology
diagnostic of breast diseases, treatment and
rehabilitation. - 2000. - Issue 3. - P.113-114.
7. Chhikvadze T.V./”Edematous breast
cancer: clinical features, diagnosis, treatment”. Russian Journal of Oncology.
2008. -N5- p.49-54.
8. Doshi A., Wedam S.B., Thomasson D.M. et al. Dynamic contrast enhanced
MRI (DCE-MRI) as a potential predictor of clinical response in patients with
inflammatory breast cancer (IBC)// ASCO Meeting Abstracts.- 2005.- V.23.-
P.584.
9. Kushwaha A.C., Whitman G.J., Stelling C.B. et al. Primary
inflammatory carcinoma of the breast: retrospective review of mammographic
findings// AJR Am J Roentgenol.- 2000.- V.174(2).- P.535-538.
10. Mogavero G.T., Fishman E.K., Kuhlman J.E. Inflammatory breast
cancer: CT evaluation// Clin Imaging.- 1992.- V.16(3).-
P.183-186.
11.Yang W.T., Le-Petross H.T., Macapinlac H. et al.
Inflammatory breast cancer: PET/CT, MRI, mammography, and sonography findings//
Breast Cancer Res Treat.- 2007. –V.109(3).-P.417-26.