P. Begun, D. Rubashova
Saint Petersburg Electrotechnical University
"LETI"
METHODS AND ASSESSMENT OF SYSTEM INTRAOCULAR PRESSURE
IN KERATOCONUS
There are several methods for measuring
intraocular pressure. The Maklakovís method is the most common in Russia. The
method of determining intraocular pressure by Maklakovís tonometer is based on
installing a particular weight with a flat surface on the eye. Under load, the
surface of the eyeball flattened by tonometerís contact surface to a certain
flattening circle. The value of the tonometric†
intraocular pressure is determined according to the diameter of the
flattening circle of corneal by the contact part of the tonometer. To converse
the tonometer readings to pressure in the unit mm Hg. Art. special calibration
tables or straightedges are required. Internals of the eyeballís structures are
not taken into account while measuring of intraocular pressure.
Numerous studies in the field of ophthalmology
has shown that the variability of the thickness and curvature of the cornea
significantly affect the results of tonometry. But, the influence of
keratoconus on the measurementís results has not been considered yet.
The corneal curvature radius and the thickness
of the central zone changes with keratoconus. Ultimately it becomes thinner and
takes a conical shape (Fig. 1). There are three stages of keratoconus:
At the first stage of keratoconus there are
reduction of visual acuity, decrease in the radius of curvature of the cornea
to 7.5-7.2 mm, decrease of the thickness of the central corneal zone to 0.48
mm;
At the second stage of the disease the
deformation of the cornea progresses, the radius of curvature decreases to
7,1-6,75 mm, the thickness of the central zone of the corneal - to 0.44 mm;
At the third stage the cornea becomes thinner,
and its radius decreases to 6,7-6,0 mm, the thickness of the central corneal
zone - to 0.40 mm.
To investigate tonometric IOP in normal and
keratoconus development model was built based on the eye orbit connective
tissue formations (Fig. 1). Tonometric IOP was calculated sequence of
iterations as a result of which the volume is not the flattened area of
the deformed eye includes an additional amount of fluid displaced
from corneal tonometer:
1.
Defined volumes: a) deformed eyes, b) aqueous humor displaced tonometer
flattened part of the eyeball, in) is not the flattened area of
the deformed eyeball;
|
|
|
Fig. 1 The scheme of the
model of the eye with the connective tissue formations orbit |
2. Conditions of zero displacement in the cornea,
in the contact zone with the tonometer, calculated displacement and deformation
is not flattened cornea and sclera;
3. Assuming a linear relationship between load
and displacement, as defined in claim 2 nonoblate character deformation of the
eye , increased its volume by 0.9 volume of fluid displaced by the tonometer;
4. Similarly, paragraph 2 provides the
equilibrium condition in the contact zone of the deformed cornea and the
tonometer;
5. Defines the scope of the non-flatness of the
eyeball;
6. If the volume is not different from the
flattened part of the original volume of the eyeball, amended in accordance
with paragraph 3 (increases or decreases the volume of the eye is not
flattened;
7. If necessary, consistently repeated the
calculations in accordance with ß 4-6.in accordance with ū. 4-6.
Research of†
keratoconusís influence on the parameters of intraocular pressure is
held with applanation load of 10 g and with the diameter of the flattening
circles are† 3, 4, 5, 6 and 7 mm.
Compliance of† the diameter of the
flattening circle and the tonometric pressure PŐ is established according to B.L. Polyakís rule.The
geometric constructions of the models were developed by the Solid Works
computer program. Stress-strain condition was calculated by Cosmos Works
finite-element software.
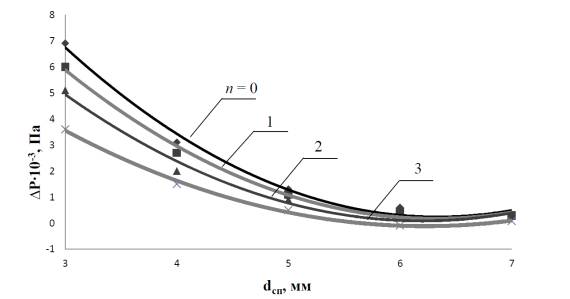
Fig. 2 shows the difference between the value
of the tonometric intraocular pressure detected by the Maklakovís method in
accordance with the rule of B.L. Polyak and tonometric intraocular pressure,
calculated according to the first model, from the diameter of the flattening
circle of the cornea in a normal state (n = 0) and at the next three stages of
keratoconus (n = 1, 2, 3).
In the study of the influence of keratoconus on
tonometry results introduced the following sumptions: 1) the material of the
cornea, sclera, dura mater, tennonovís capsules, fasciae musculares materials,
episcleral space and orbital bones is uniform, solid and isotropic with† reduced modulus of resilience; 2) the model
is rigidly fixed on the outer side of the eye socket bone; 3) modulus of
resilience of the cornea EP = 0.362 MPa, modulus of resilience the
contact part of the tonometer ET = 210 GPa; reduced modulus of
sclera, dura mater, tennonovís capsules, resilience fasciae musculares,
episcleral space and orbital bones are equal respectively EC = 6
MPa; ETMO = 150 MPa; E“ = 200 MPa;† ECT = 20 MPa,† E›= 30 kPa, E = 2.5 GPa. 4) the radius of curvature of the cornea
in a normal state (n = 0) R – = 7.8 mm, the
central zone thickness h–÷ = 0,52 mm, thickness
at the periphery of the cornea assumed to be constant at all stages of† keratoconus h–Ō = 0.6 mm. At the next three stages (n = 1, 2, 3)
cornea changes its curvature R – = 7.2 mm (n = 1),
6.8 mm (n = 2) and 6.2 mm (n = 3) and central†
zone thickness, respectively h–÷ = 0.48 mm, 0.44 mm
and 0.4 mm; thickness and radius of curvature of the sclera HC = 0.7
mm RKC = 12 mm, diameter dura mater DH = 2.1 mm; the
thickness and radius of curvature tennonovís capsule HTK = 0.74 mm,
RTK = 13 mm; dimensions fasciae musculares T—“ = 5 mm, t—T1 = 11.25 mm, t—T2 = 16 mm, h—T1 = 0.7 mm, h—T2 = 1.76 mm, outer diameter
fasciae musculares d—T = 36.7 mm, height
of the orbit Õ√ = 52.5 mm outer
diameter orbit D√ = 49 mm, inner
diameter of the orbit d√ = 33 mm.
|
|
|
Fig.
2. The dependence of the difference between the value of the tonometric
intraocular pressure detected by the Maklakovís method in accordance with the
rule of B.L. Polyak and tonometric intraocular pressure, calculated according
to the fourth model, from the diameter of the flattening circle. |
The model is divided into 70000 tetrahedral
finite elements. With the increasing of the stage of keratoconus development
Corneal of the eye becomes more pliable. When flattening circles are from 7 mm
to 3 mm, intraocular tonometric pressure increases relative to the norm from
10, 8% to 37.3%. With the increasing of the stage of keratoconus's development
the discrepancy of calculated tonometric intraocular pressure and tonometric
intraocular pressure detected by the Maklakovís method decreases.