Медицина/ 7.Клиническая медицина.
Zhaisakova
D.E., Kaltayeva M.B.
Asfendiyarov Kazakh National Medical University, Department of Otorhinolaryngology,
Kazakhstan.
The study of sensorineural hearing loss etiological structure.
The problem of hearing loss is still relevant in the medical and social terms, as
it often leads not only to a significant life quality deterioration, but also
causes disablement in a number of patients.
The identification of the hearing loss causes is the main stage on the way
of solving problems related to the search for effective methods of inner ear
diseases treatment. Whereas, genetic disorders were deemed to be the cause of
60% of all congenital and early pediatric hearing loss cases. [1; 2]. About 2/3
(66%) of nonsyndromic hearing impairments are of genetic origin, while 1/3
(33%) are associated with environmental factors [3, 5].
In 2005, R. Smith
published an article, which contains the diagram demonstrating data on
syndromic and nonsyndromic forms of hearing loss according to its share in the
general group of congenital and prelingual pediatric hearing loss cases (Pic.
1) [24;5].
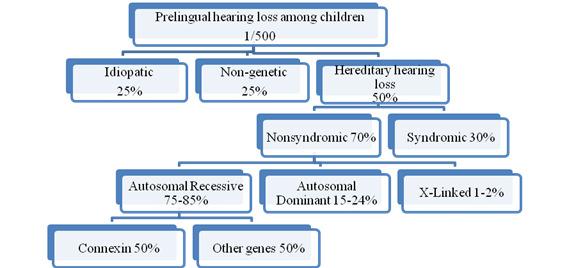
Picture 1. Summary of congenital and
prelingual hearing loss genetic characteristics according to R.Smith and Guy Van Camp [24; 5].
According to Figure 1, created by R. Smith and Guy Van
Camp, 50% of all congenital and prelingual hearing loss has an acquired
character. The rest cases occur due to genetic changes. Hereditary hearing loss
include up to 30% syndromic forms and 70% of nonsyndromic forms of hearing
impairments. It is believed that the latter include 75% -85% autosomal
recessive forms, 15% -24% autosomal dominant forms, 1-2% X-linked recessive
forms, and 1% was associated with
mitochondrial DNA mutations. Autosomal recessive nonsyndromic hearing
loss forms in 50% of cases are linked with the DFNB1 locus (Cx26 and Cx30
genes). Thus, the Cx26 gene mutation amounts not less than 16% of all
prelingual SNHL cases. The remaining 50% are associated with the other
recessive loci [5].
The development of hearing
pathology is influenced by various causes. It has been established that the causes include violations in the antenatal
- prenatal period (marriage between close relatives, rubella, syphilis,
metabolic disorders, drugs with ototoxic effect), perinatal period (birth
trauma - anoxia, jaundice (hemolytic), drugs with ototoxic effect) and neonatal
- postnatal period (otitis media, infectious diseases (meningitis,
measles, parotitis), trauma of the cervical spine and head, drugs with ototoxic
effect) (Yu.V. Kozyun, G.A. Tavartkiladze).
According to various authors, the
acquired hearing loss in children most commonly occurs as a result of prenatal
infections such as toxoplasmosis, rubella, cytomegalovirus, and herpes. In
this regard, in recent years there has been a significant increase in interest
in the problem of prenatal infections, among which a special attention has been
paid to herpesvirus infections and, in particular, cytomegalovirus infection. Herpes
and cytomegalovirus infections remain one of the leading causes of stillbirth,
spontaneous miscarriages, premature births, neonatal morbidity and infant
mortality. According to the data of domestic and foreign specialists, from 0.5
to 5% of children are born with congenital CMV (cytomegalovirus) infection,
about 90% of which of are asymptomatic carriers children [8; 7]. At the same
time, the subclinical form of CMV infection does not mean a guarantee of
well-being, violations of central nervous system, hearing, vision, cerebral
palsy, mental retardation, poor school performance are diagnosed in 5-15% of
such children in the next 1-2 years and later [9;10]. And also high incidence of Down's
disease is associated with congenital CMV infection [11]. Many surviving children
have long-term and sometimes lifelong complications: 28% have a mental
retardation, 58% have neuromuscular disorders, including cerebral palsy, as
well as somatosensory insufficiency, 20% have hearing loss, 24% have visual
impairment [11]. All this led the European Regional Bureau of the World
Health Organization to the decision to include CMVI (cytomegalovirus infection)
in a group of diseases that determine the future of infectious pathology in
1984 [11]. In addition, WHO included CMVI in intrauterine infectious disease
syndrome called TORCH syndrome, which includes T-toxoplasmosis, O-syphilis,
listeriosis and other infections, R-rubella, C-cytomegalovirus infection and
chlamydia, H-herpes and hepatitis [11].
According to the large-scale study conducted by the researchers of the Research
Institute of Obstetrics and Gynecology of the Republic of Kazakhstan, primary
CMV infection was detected in 31.2% of women with threatened miscarriage, in 18.2%
of women with a spontaneous abortion, in 39.5% of women with premature birth,
at 53.4% of women with polyhydramnios, in 35,4% of women with missed
miscarriage [11].
And also premature birth, low body weight,
child asphyxia refer to important exogenous risk factors.
In the total population of newborns, the share of premature infants is
becoming more and more significant and amounts to 5-10% of newborns [19]. According
to studies conducted in France and the United States, the incidence of severe
hearing impairment in the group of newborns with a body weight of less than
2000g is 15.5 per 1000, and in the group of small premature infants it is 4-5%
[20]. In recent years, the importance of perinatal pathology has significantly
increased as one of the causes of congenital hearing loss and deafness in
children [22,23]. In addition, it is known that this pathology develops in the
first year of life in 82% of children with hearing loss and deafness, and in
38.5% of them - in the perinatal and neonatal period [21].
Postnatal
infections, in particular, bacterial meningitis caused by Neisseria
meningitidis, Haemophilusinfluenzae, Streptococcus pneumoniae, are often
complicated by total hearing loss, vestibular disorder [5].
Meningitis continues to be one of the most common forms of damage to the
central nervous system (neuroinfections) in adults and children worldwide. Depending
on the pathogens, all cases of diseases are usually subdivided into bacterial
(purulent) and viral (serosal) meningitis [4]. According to
the World Health Organization, around 1 million cases of bacterial purulent
meningitis are registered worldwide annually, 200 thousand cases of which are
fatal cases [12,13]. Meningitis is one of the most frequent clinical forms in
the structure of the general pathology of the nervous system [13; 17].
In the
Republic of Kazakhstan, meningococcal infection is more often diagnosed in
children. According to official statistics of the Republic of Kazakhstan, the
highest incidence rate was registered in Almaty city (1.58 per 100 thousand
people in 2012) and in Astana city (1.38 per 100 thousand people in 2012) [18].
Currently,
despite the reduction in morbidity, the level of lethality remains high. Children
of Almaty were conducted a study on the clinical and epidemiological features
of meningococcal infection at the present stage in 2009-2013, which goal was to
assess the incidence of generalized forms of meningococcal infection in
children at the age of 0-14 years, assess the distribution of Neisseria meningitides serogroups in children
patients, estimate the proportion of meningococcal meningitis and meningitis of
unclear etiology in the overall structure of bacterial meningitis and to
estimate the frequency of treatment in the intensive care unit, the incidence
of complications, mortality. The study revealed that within five years the
incidence of meningococcal infection ranged from 5.7 per 100 thousand people to
14.7 cases per 100 thousand people. These data exceeded the official figures
twice. The lowest incidence was observed in 2009, the highest in 2012. This
demonstrates the wave character of the epidemiological process of meningococcal
infection, which makes it possible to predict an increase in the incidence rate
in the next two years [18].
The patients
were mostly children under the age of 5, with the highest incidence rate in
children under 1 year old. In general, if we speak about all purulent bacterial
meningitis cases, then there is no tendency to reduce the incidence rate for
the period 2009-2013. Meningococcal meningitis (32%) prevailed in the etiologic
structure of the children's population of Almaty (1993-2007) and unfortunately
a percentage of meningitis of unknown etiology was remaining high (39,8 %)
[18]. There is a high mortality rate in purulent meningitis, reaching an
average of 4-10%, which is due to the severity of the course and numerous
complications of the disease. They include: toxic shock syndrome (TSS),
hypertension-hydrocephalic syndrome (HHS), sensorineural hearing loss syndrome,
development of paresis and paralysis, apallic syndrome. Persistent organic
lesions of the central nervous system (CNS) in the residual period are observed
in almost 1/3 of the children who have recovered from the disease [16, 14,
15, 13].
For a long time, hearing loss was considered
to be acquired as a result of ototoxic antibiotics effect. The existence of a
hereditary predisposition to the effects of the ototoxic drugs is no longer in
doubt. Isolated hearing loss develops when there is a mutation in the gene
encoding the 12S protein of ribosomal RNA of mitochondrial DNA. But, the onset of hearing loss with this
mutation may also be related to the effect of ototoxic drugs. Carriers of the
mutation in 12S gene of ribosomal RNA of isolated hearing loss development are
enough smaller doses of aminoglycosides [5, 26].
Numerous studies indicate a significant
contribution of genetic factors in violations of auditory perception. The
absence of data on cases of hearing impairment among family members does not
exclude the possibility of the genetic origin of hearing loss, but one can also
expect the acquired character of the lesion in a child from deaf parents.
References:
1. Smith RJ. Clinical application of
genetic testing for deafness/ R J. Smith //Am. J. Med. Genet.
A.-2004.-Vol.l30.-P.8-12.
2. Finsterer J. Nuclear and mitochondrial genes mutated in nonsyndromic
impaired hearing / J.Finsterer, J.Fellinger // Int. J. Pediatr.
Otorhinolar.-2005.-Vol.69.- P.621-647.
3. Waardenburg P.J. A new syndrome combining developmental anomalies of
the eyelids, eyebrows, and nose root with pigmentary defects of the iris and
head hair and congenital deafness / P.J.Waardenburg //Am. J. Hum.
Genet.-1951.-VoL3. - P.
195-253.
4. Pepys M.B., Hirschfield G.M. C-reactive
protein: a critical update. // J. Clin. Invest. 2003. - V. 111, N12. - P.
1805-1812.
5. Markova T.G. Clinical and genetic analysis of
congenital and prelingual hearing loss, Author's Abstract of Doctor of Medicine, Moscow2008, p. 24-37.
8. Kenneson
A, Cannon MJ. Review and meta-analysis of the epidemiology of congenital
cytomegalovirus (CMV) infection. // Rev Med Virol. 2007 Jul-Aug; 17(4)- P.253-76.
9. Michaels
MG. Treatment of congenital cytomegalovirus: where are we now? Expert Rev Anti Infect
Ther. 2007 Jun;5(3)- P.441-448.
10. Pavlova
M.V. Diagnosis of cytomegalovirus infection in preterm newborns and evaluation
of anti-CMV activity of new membrane-polyanionic compounds in vitro. / /
Author's Abstract, Candidate of Medicine, Moscow 2008, P. 21-23.
11. A.S. Aidarbekova LM, Duysenbieva et.al. Cytomegalovirus infection in
pregnant women, the risk of complications in the perinatal period. MEDICINE, №4, 2014, page 59.
12. Clinical predictors for hearing loss in children with bacterial
meningitis / J. Kutz, L. Simon, S. Chennupati et al. // Arch, of Otolaryngology
-Head & Neck Surgery. 2006. - Vol. 132, №9. - P. 941-945.
13. Makarova Т.Е. Scientific substantiation of pathogenetic therapy of bacterial
purulent meningitis. Author's abstract. Doctor of Medicine. 14.00.09 Khabarovsk-2012,
p.10-11.
14. Kozlov, V. Immunopathogenesis and cytokine therapy of surgical
sepsis / V. Kozlv. SPb, 2002.- Р.48.
15. Complex investigation of the phagocytic link of immunity in primary
immunodeficiency states / M. 3. Saidov, LA Gomes, MN Yartsev et al., The
Journal of Microbiology, epidemiology and immunobiology. -1991.-№5.- P. 44-46.
16. Clinic, diagnosis and treatment of H1b meningitis in children / RN
Bykova, IS Koroleva, Yu. Ya. Vengerov et al.// Infectious diseases. 2007. - №4.- P. 32-36.
17. Gerasimov, IG Kinetics of the Reaction of the
Restoration of Nitrosine Tetrazolium by Human Blood Neutrophils / IG Gerasimov,
OA Kalutskaya // Cytology. 2000. - Т. 42, No.2. - P. 160-165.
18. Eralieva
L.T. Meningococcal
infection in children at the present stage: changes and possibilities of
fighting it. Health of Kazakhstan. No.2/56, March 2017, p 27‑29.
19. Zagoryanskaya M.E., Rumyantseva M.G. "Opportunities for Early Rehabilitation of
Children with Hearing Impairment" Russian Otorhinolaryngology Appendix №1 - 2008 - p.257-261.
20. Sun J.H.,
Li J., Huang P., Bu J., Xu Z.M., Li J., Shen X.M. «Early detection of hearing
impairment in high-risk infants of NICU» Zhonghua-Er-Ke-Za-Zhi. 2003 - May -
41(5)- Р. 357-358.
21. Kozun
Yu.V., Kibchenko S.I. "Methodical approaches to the assessment of the
state of the auditory analyzer in children of the first years of life"
"Bulletin of Russian State Medical University" - 2000 – 2 (12) - Р. 115.
22. Otvagin I.V. Epidemiological study of the etiological factors of
hearing impairment in children of the younger age group of the Central Federal
District // Russian otorhinolaryngology. №1, 2005, p. 140-142.
23. Starokha AV,
Khandazhapova Yu.A., Davydov AV, Khabas MV, Madison AE, Litvak M.М. "The first experience of total audiological screening of
newborns" Materials of the 2 nd National Congress of Audiologists, 6th
International Symposium.
24. Smith R.J. Sensorineural hearing
loss in children / RJ.Sinilb, J.F.BaleJr, K.K.
White //Lanoet.-2005.-Voi .365 .- P.879 - 890.
25. Steel K.P. A genetic approach to understanding
auditory function / K.P.Steel, C.J.Kros //Nature Genet.- 2001.-Vol.27.-P. 143-149.
26. Stevenson
V.A. Connexin-30 deletion analysis in connexin-26 heterozygotes /V.A.Stevenson,
M.Ito, J.M.Milunsky // Genet Test.-2003.-Vol.7.-P. l51-154.