P.I. Begun, E.A.
Lebedeva, D.A. Rubashova, O.V. Shchepilina
Saint Petersburg
Electrotechnical University "LETI", St. Petersburg, Russia
BIOMECHANICAL SIMULATION IN MEDICAL
PRACTICE
Summary
The questions connected
with biomechanical simulation in medical practice are considered. The leading
role in biomechanical investigations is played by integral computer method.
Considered method is a combination of biomechanical computer simulation and the
analysis of biological structures according to the results of clinical (tomography, angiographic,
echographic) investigations.
Keywords: biomechanics, simulation, medical practice, finite element
package, tomography, angiographic, echographic.
I. Introduction. Introduction into medical practice
of new prosthesis methods and assessment of methods of diagnostics is connected
with the necessity of enlargement and enrichment of information implementation
on wider scale. The absence of necessary information provides objective
difficulties and does not allow to plan
the success and forecast the result of the operation done technically
correctly. In all the basic spheres of the task: medical, technical and
fundamental the simulation on the basis of biomechanics of biological object –
prosthesis is integral. And the construction of the models of the human body
parts functioning in normal state, when pathology and while prosthsesing
greatly depends on the use of all the set of new methods and means of investigations.
The leading role in biomechanical investigations is played by integral computer
method. This method is a combination of biomechanical computer simulation and
the analysis of biological structures according to the results of clinical
(tomography, angiographic, echographic) investigations. The complexity of
geometrical shapes of investigated biological objects, their inhomogeneity and
anisotropy of their structural mechanical properties predetermined the
construction of mathematical models in the frames of three-dimensional body
mechanics and parametric models built in finite element package Solid Works,
Cosmos Works, NASTRAN, COMSOL, ANSYS. Interactive software package Mimics
allows to visualize and segment the images
received with the help of tomography and
construct biological objects
on the base of tomography.
II. Problem definition. The simulation process consists of
the allocation of object’s properties and its
interaction with other objects, the notification of the peculiarities in
functioning in different external influences and logic analysis of the
information received. The model is a
speculative idea of a real object which reflects the characteristics of the real
object which are necessary to get
an answer to the given task.
The usage of computer
programs based on numerical methods allows to delve into the fields which
cannot be served by analytical methods due to large complications in
implementation. Analytical approach and the computer numerical method are
interpenetrative and supplemental each other methods. With powerful software numerical computer analysis takes up
dominant position.
Physical modeling is
based on reproduction of biotechnical objects, functions and processes with
physical methods. Physical modeling allows to replace investigation of a real object
by the research of
characteristics of reduced or increased
mechanically similar model with the following transition from the model
parameters to the corresponding parameters of biotechnical object. The scientific
base of physical modeling is the similarity theory. The methods of
similarity theory allow to transfer
from reference physical values to some
generalized variables – similarity criterion. This allows to decrease
the quantity of physical parameters describing the phenomena and get a large
alliance of the received result.
Modeling process consists of allocation of characteristics of
the object and its interaction with other objects, reflection of peculiarities
in functioning at different external influences and logic analyses of gathered
information.
The model reflects the
structure and function of the original system by means of structure and
functions of those elements it is built of.
III. Results. We will illustrate told above on examples.
Example A. Modern
problems of rehabilitation after hip fracture due to the fact that is not
governed by the maximum load, taking into account the recovery of bone
regenerate and is not considered a risk of vascular disorders. At the same time
during postoperative period after the hip fracture results from the fact that
the thighbone traumatic injury affects the locomotor system kinematic reactions
in general, thus facilitating associated disorders that do not directly result
from the injury, yet worsening the patient’s life.
Despite new implant
designs, improved skills of surgeons, new operation methods implemented, the
results stop satisfying patients as the full recovery period reaches half a
year. This is because the missing is the individual approach depending on the
bone tissue condition, the fracture location. The issue of the bone graft
reconstruction at the subcapital fracture location lacks attention.
However, information
technologies development in medicine, particularly in trauma surgery,
orthopedics and biomechanics allows achieving radically new rehabilitation
technology level.
The object of the
research is to develop thighbone diagnostic technique after osteosynthesis with
muscle activity and elasticity module (E, MPa) taken into account at every bone
graft remodeling stage. The algorithm has been developed, the calculations have
been carried out and the analysis and the research have been undertaken for the
“thighbone-bone graft-implant” system stress and stain behavior at various
rehabilitation stages.
The following assumptions
were considered while building the conceptual model:
1) thighbone bone
structure is idealized to comprise two isotropic layers: cortical and spongy;
2) within the thighbone,
the fissure is located at the thighbone neck cross-section and it has uniform
isotropic structure, wherein its mechanical properties change at every
osteotylus reconstruction stage and those are localized within the zone that is
free of muscular efforts;
3) dynamic stress is
applied to the thighbone center by axes X, Y, Z (www.orthoload.com).
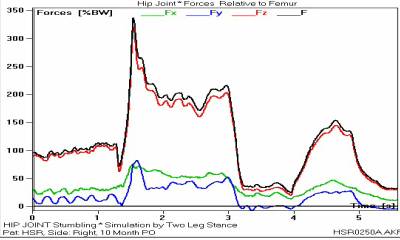
Figure 1 represents
experimental data, with the coordinate system selected axes orientation and
coordinate center within the thighbone shown (a), as well as the example of the
effective load changes as a function of time (b).
|
a |
b |
|
|
|
|
Fig.1. Test data |
|
As initial data, the
thighbone MRT is used to build the object 3d models by means of Mimics, the
computer modeling environment. With those models imported into the Solid Works
software package, a solid thighbone geometric model was obtained with damages at
the area of the greater trochanter. The considered is the bone recovery via
osteosynthesis, with two cannulated titanium screws.
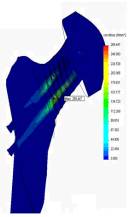
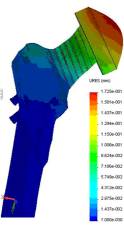
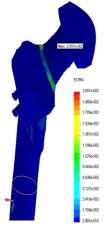
In terms of non-linear
dynamic analysis, various rehabilitation procedures, relating to the first two
rehabilitation stages, were considered. The obtained results are represented
via fig.2. Figure 2 represents the
stress diagram (a), displacement (b), deformations (c) to the femur at the hip
abduction in the side in a sitting position and represents dependences of
deformations appearing at the first stage with Eper=5.4kPa ( d): 1 –
allowed deformation, 2 – deformation with the thigh aside, 3 – deformation for
the thigh up 30°.
|
a |
b |
c |
d |
|
|
|
|
|
|
Fig.2. The first stage
of rehabilitation |
|||
The following was
concluded there from:
1) the tendency was
discovered of the deformation depending on the elasticity module E, thus this
factor must be taken into consideration when developing rehabilitation
programs, particularly for the initial stages of the rehabilitation, when the
bone structure has not fully restored after the damage yet, and the blood
vessels are vulnerable for significant deformations;
2) putting a thigh aside
during the first stage of rehabilitation, as well as walking with support on
the bad leg are counter-indicative for patients with the subcapital fracture who underwent osteosynthesis.
Example B. There are
several methods for measuring intraocular pressure. The Maklakov’s method is
the most common in Russia. The method of determining intraocular pressure by
Maklakov’s tonometer is based on installing a particular weight with a flat
surface on the eye. Under load, the surface of the eyeball flattened by
tonometer’s contact surface to a certain flattening circle. The value of the
tonometric intraocular pressure is determined according to the diameter of the
flattening circle of corneal by the contact part of the tonometer. To converse
the tonometer readings to pressure in the unit mm Hg. Art. special calibration
tables or straightedges are required. Internals of the eyeball’s structures are
not taken into account while measuring of intraocular pressure. Numerous
studies in the field of ophthalmology has shown that the variability of the
thickness and curvature of the cornea significantly affect the results of
tonometry. But, the influence of keratoconus on the measurement’s results has
not been considered yet. The corneal curvature radius and the thickness of the
central zone changes with keratoconus. Ultimately it becomes thinner and takes
a conical shape (Fig. 3).
|
|
|
Fig. 3. The scheme of the model of
the eye with the connective tissue formations orbit |
There are three stages of
keratoconus: at the first stage of keratoconus there are reduction of visual
acuity, decrease in the radius of curvature of the cornea to 7.5-7.2 mm,
decrease of the thickness of the central corneal zone to 0.48 mm; at the second
stage of the disease the deformation of the cornea progresses, the radius of
curvature decreases to 7,1-6,75 mm, the thickness of the central zone of the
corneal - to 0.44 mm; at the third stage the cornea becomes thinner, and its
radius decreases to 6,7-6,0 mm, the thickness of the central corneal zone - to
0.40 mm.
To investigate tonometric
IOP in normal and keratoconus development model was built based on the eye
orbit connective tissue formations (Fig. 3). Tonometric IOP was calculated
sequence of iterations as a result of which the volume is not the flattened
area of the deformed eye includes an
additional amount of fluid displaced from corneal tonometer:
1. Defined volumes: a)
deformed eyes, b) aqueous humor displaced tonometer flattened part of the
eyeball, in) is not the flattened area of the deformed eyeball;
2. Conditions of zero
displacement in the cornea, in the contact zone with the tonometer, calculated
displacement and deformation is not flattened cornea and sclera;
3. Assuming a linear
relationship between load and displacement, as defined in claim 2 nonoblate
character deformation of the eye , increased its volume by 0.9 volume of fluid
displaced by the tonometer;
4. Similarly, paragraph 2
provides the equilibrium condition in the contact zone of the deformed cornea
and the tonometer;
5. Defines the scope of
the non-flatness of the eyeball;
6. If the volume is not
different from the flattened part of the original volume of the eyeball,
amended in accordance with paragraph 3 (increases or decreases the volume of
the eye is not flattened;
7. If necessary, consistently
repeated the calculations in accordance with § 4-6.in accordance with ð. 4-6.
Research of keratoconus’s
influence on the parameters of intraocular pressure is held with applanation
load of 10 g and with the diameter of the flattening circles are 3, 4, 5, 6 and 7 mm. Compliance of the diameter of the flattening circle and
the tonometric pressure PÌ is established according to B.L. Polyak’s rule.The
geometric constructions of the models were developed by the Solid Works
computer program. Stress-strain condition was calculated by Cosmos Works
finite-element software.
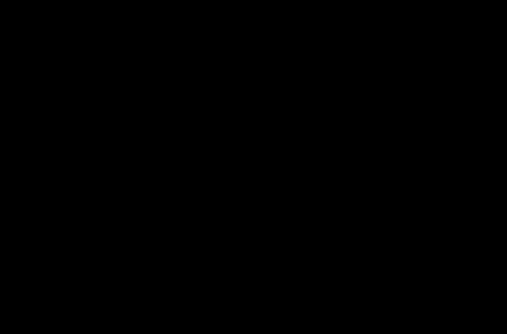
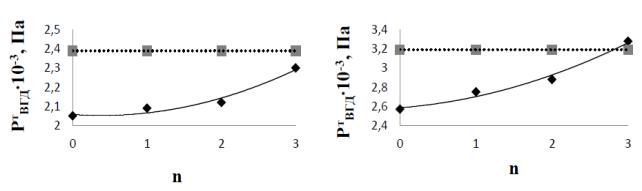
Fig. 4 shows the
calculation results of tonometric intraocular pressure for the model at three
stages of keratoconus (n = 1, 2, 3).
|
a |
b |
|
|
|
|
Fig.
4. The dependence of the investigated
tonometric intraocular pressure (slanting line) and intraocular pressure
detected by the Maklakov’s method in accordance with the rule of B.L. Polyak
(horizontal line) from the stage of keratoconus calculated according to the
model, flattening circle diameter of 7 mm (a) and 6 mm (b). |
|
In the study of the
influence of keratoconus on tonometry results introduced the following
sumptions: 1) the material of the cornea, sclera, dura mater, tennonov’s
capsules, fasciae musculares materials, episcleral space and orbital bones is
uniform, solid and isotropic with
reduced modulus of resilience; 2) the model is rigidly fixed on the
outer side of the eye socket bone; 3) modulus of resilience of the cornea EP
= 0.362 MPa, modulus of resilience the contact part of the tonometer ET
= 210 GPa; reduced modulus of sclera, dura mater, tennonov’s capsules,
resilience fasciae musculares, episcleral space and orbital bones are equal
respectively EC = 6 MPa; ETMO = 150 MPa; EÒÊ = 200 MPa; ECT = 20 MPa, EÝ= 30 kPa, EÊ = 2.5 GPa. 4) the radius
of curvature of the cornea in a normal state (n = 0) RÊÐ = 7.8 mm, the central
zone thickness hÐÖ = 0,52 mm, thickness at the periphery of the cornea assumed
to be constant at all stages of keratoconus
hÐÏ
= 0.6 mm. At the next three stages (n = 1, 2, 3) cornea changes its curvature RÊÐ = 7.2 mm (n = 1), 6.8 mm
(n = 2) and 6.2 mm (n = 3) and central
zone thickness, respectively hÐÖ = 0.48 mm, 0.44 mm and 0.4 mm;
thickness and radius of curvature of the sclera HC = 0.7 mm RKC
= 12 mm, diameter dura mater DH = 2.1 mm; the thickness and
radius of curvature tennonov’s capsule HTK = 0.74 mm, RTK
= 13 mm; dimensions fasciae musculares TÑÒ = 5 mm, tÑT1 = 11.25 mm, tÑT2 = 16 mm, hÑT1 = 0.7 mm, hÑT2 = 1.76 mm, outer
diameter fasciae musculares dÑT = 36.7 mm, height of the orbit ÍÃ = 52.5 mm outer diameter
orbit DÃ
= 49 mm, inner diameter of the orbit dà = 33 mm.
The model is divided into
70000 tetrahedral finite elements. With the increasing of the stage of
keratoconus development Corneal of the eye becomes more pliable. When
flattening circles are from 7 mm to 3 mm, intraocular tonometric pressure
increases relative to the norm from 10, 8% to 37.3%. With the increasing of the
stage of keratoconus's development the discrepancy of calculated tonometric
intraocular pressure and tonometric intraocular pressure detected by the
Maklakov’s method decreases.