Êëèíè÷åñêàÿ
ìåäèöèíà
Prof. Semenov V. A., prof. Subbotin A. V.
Kemerovo State Medical Academy
Magnetic
resonance imaging in patient with chronic tick-borne encephalitis and early
manifestation of convulsion-hyperkinetic disorder
Currently,
chronic tick-borne encephalitis is a poorly understood phenomenon. There are virtually
no clinical data on its early manifestations as well as data obtained from
advanced neuroimaging techniques [1].
Material and
methods
A rare case of chronic
tick-borne encephalitis in vaccinated patient is presented. The patient N was
born in 1961, was immunized twice (0.5 ml, FSME-Immun, series AB) against
tick-borne encephalitis on 01.10.2009 and 25.02.2010. Acute disease: the
infectious syndrome developed on 25.07.2010; the patient was admitted to the
hospital on 27.07.2010, the in-hospital period was 46 days; timely outpatient
follow-up is currently performed. Neurological status was assessed in the acute
phase of the disease: peripheral paresis of the proximal left upper extremity
nerves, 1-2 scores; tremor of the upper extremities. Discharge diagnosis:
tick-borne encephalitis, meningoencephalitis, subcortical and cerebellar
syndrome. The patient is in satisfactory condition.
Outpatient follow-up
period between 2010 and 2014. The patient has a tremor of the upper
extremities; high titers of tick-borne encephalitis virus-specific IgG
antibodies are present in the samples.
EEG, performed on
06.09.2013. Short-term aperiodic oscillations formed high-amplitude sharp waves
with deformed theta and delta slow wave activity in the frontal, temporal and
parietal regions of the right hemisphere of the brain were recorded. Chronic tick-borne
encephalitis, the onset of convulsion-hyperkinetic syndrome were diagnosed [2].
Magnetic
resonance imaging (MRI) of the brain was acquired on a Siemens HARMONY 1,0T
(23.08.2010), a Philips Achieva Nova 1,5T (02.11.2013), GE Brivo MR355 1,5T
(03.12.2013) using the standard protocol, including T1- and T2- - weighted sequences
and inversion recovery (IR).
Bioelectric brain
activity was measured by electroencephalography (EEG). EEG electrode setup
internationally standardized 10-20 system with bipolar and uninopolar
measurements. EEG recording was carried out on 17-channel electroencephalograph
“Nihon Konden” (Japan) using the software “NeuroCheck”, allowing the
calculation of the spectrum signals using the fast Fourier transform for 1-16
second epochs with digital band-pass filtering, including the efficient amplitude
detection and measurement in 4 frequency bands (delta, theta, alpha, beta).
Immunological
studies of blood and cerebrospinal fluid to verify the causative agent were
performed by ELISA in the Immunology Laboratory of the Kemerovo Regional
Clinical Hospital, using test systems “Vector-Best” (Novosibirsk) Vecto-TBE-IgM,
series 123, and Vecto-TBE-IgG, series 131.
Results and Discussion
The brain MRI,
performed in the subacute phase of tick-borne encephalitis (23.08.10), revealed
asymmetric, predominantly left-sided multifocal white matter lesions (up to 5
foci) of hyperintense signal on T2WI and TIRM, of iso- to hypointense on T1WI,
localized predominantly periventricular to posterior horns of the lateral
ventricles. The foci sizes ranges from 0.5 cm to 1.0 cm with a small perifocal
edema. The signs of paravasal microcirculatory disorders associated with
dilated Virchow-Robin spaces in the white matter of both hemispheres have been
found in the basal structures (globus pallidus, inferolateral fibers of the
internal capsule) to a lesser extent. Small areas of gliosis have been observed.
There were no focal changes on DWI (b = 500, b = 1000), ADC mapping.
Follow-up MRI
(2013) revealed indirect signs of intracranial hypertension: enlarged perioptic
subarachnoid spaces without cerebral cavity expansion; there were no signs of
brain atrophy. Within the white matter of the brain (posterior watershed zone),
both on the right and on the left sides (Fig. 1, 2), T2 / FLAIR hyperintense
small foci, located in the juxtacortical, subcortical and deep white matter
areas (the border zone) have been found; another similar focus has been visualized
juxtacortical in the front insular region on the left. The foci were rounded or
spindle-shaped with the radial type of location perpendicular to the boundaries
of the lateral ventricles. There were no signs of pathological accumulation of
gadolinium - containing contrast agent after its administration. The number of
foci as well as their sizes and shapes did not undergo any significant
transformation. Due to cumulative signs the referred foci probably belong to
the perivascular domain, suggesting infectious / inflammatory etiology for
these lesions [3].
A comparison of
the obtained data with the available brain MRI findings in tick-borne encephalitis,
indicating the presence of foci of neuronal inflammatory degradation of the
central nervous system with reactive astrocytosis and neuronophagia [4,5], is
consistent with the descriptions of pathological changes typical perivascular
infiltrates with multifocal neurodegeneration and gliosis in chronic tick-borne
encephalitis [6].
The presented MRI
findings of the changes in the brain correspond to the manifestations of
chronic tick-borne encephalitis.
\\\\
References:
1. Khafizova
I.F., Yakupov E.Z., Matveeva T.V. et al. Chronic encephalitis with disseminated
encephalomyelitis (case report). // Journal of Neurology and Psychiatry in
2012, ¹9, Issue 2, P.48-51
2 Subbotin A.V.
Prognostic methods for chronic encephalitis with Kozhevnikov epileptic syndrome
SU 1806599 A1
3. S. Medrano
Martorell, M. Cuadrado Blazquez, D. Garcia Figueredo, S. Gonzalez Ortiz, J.
Capellades Font // Hyperintense punctiform images in the white matter: A
diagnostic approach // Radiologa. 2012; 54 (4): R.321-335
4. Alkadhi H,
Kollias SS. MRI in tick-borne encephalitis. // Euroradiology. 2000 Oct; 42
(10): 753-5.
5. Marjelund S,
Tikkakoski T, Tuisku S, Räisänen S. Magnetic resonance imaging
findings and outcome in severe tick-borne encephalitis. Report of four cases
and review of the literature. // Acta Radiol. 2004 Feb; 45 (1): 88-94.
6. Shapoval A.N.
Tick-borne encephalomyelitis. M., Med. 1980. – 255 p.
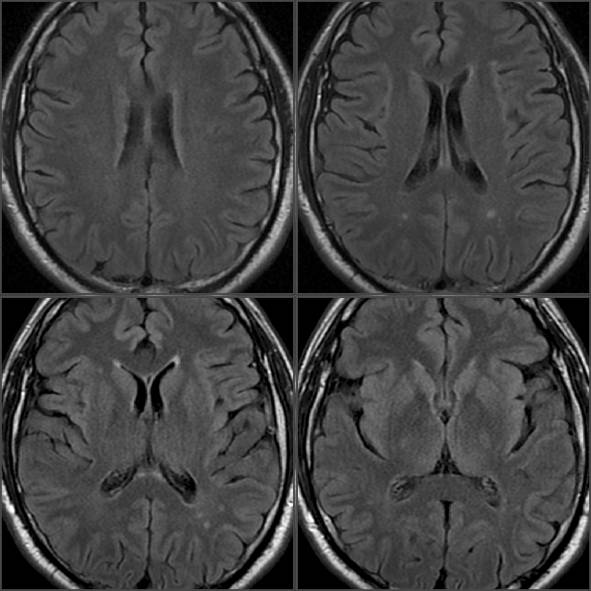
Fig. 1
Supratentorial axial T2 FLAIR - weighted, slice thickness 5 mm.
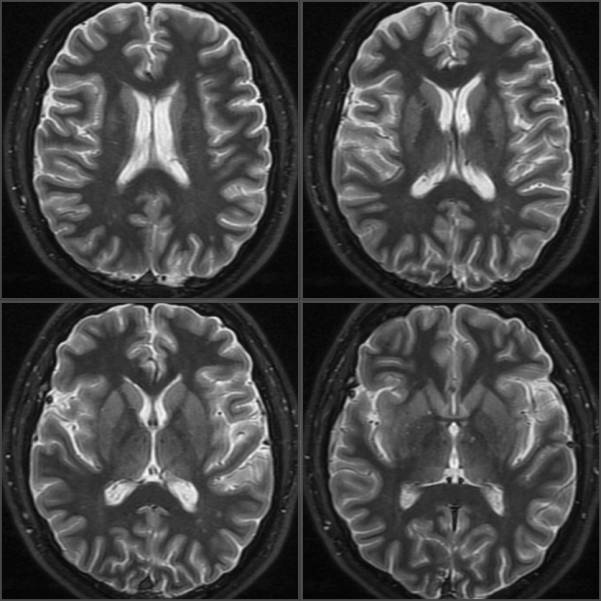
Fig. 2
Supratentorial axial T2 irFSE - weighted, slice thickness 4 mm.
Authors
1 Vladimir A.
Semenov – MD., PhD., Professor, FSBEI HPE “Kemerovo State Medical Academy of
the Ministry of Health of the Russian Federation” (Kemerovo)
2 Anatoly V.
Subbotin – MD., PhD., Professor, the Head of the Neurology, Neurosurgery and
Medical Genetics Department at the FSBEI HPE “Kemerovo State Medical Academy of
the Ministry of Health of the Russian Federation” (Kemerovo)
Key Words
Chronic tick-born encephalitis, MRI.
Abstract
The MRI findings
of the early onset of chronic tick borne encephalitis with
convulsion-hyperkinetic syndrome in a vaccinated patient are presented.
Figure notes:
Fig. 1
Supratentorial axial T2 FLAIR - weighted, slice thickness 5 mm.
Fig. 2 Supratentorial
axial T2 irFSE - weighted, slice thickness 4 mm.