Some parameters hemostasis and endothelial dysfunction in patients
with diabetic macular edema and diabetes mellitus type 2
Shelkovnikova T.W., Takhchidi Kh.P.,
Katsadze Y.L., Shishlyannikova N.Y.
Kemerovo, Kemerovo Oblast Clinical
GBUZ Eye Hospital
Moscow, Russian State Educational
Institution National Research
University of Pirogova
St. Petersburg, Federal Russian
Institute of Hematology and Transfusion,
Kemerovo, Kemerovo State Medical
Academy Russian Ministry of Health
Purpose: study of some parameters of
hemostasis, endothelial dysfunction, hereditary thrombophilia markers, clinical
and morphological parameters of macular edema in patients with diabetic
retinopathy (DR) and diabetes mellitus type 2 (DM 2).
Materials and methods: 50 patients (100 eyes) with DR-2
diabetes. Of these, the nonproliferative diabetic retinopathy (NPDR) - 12
patients (24 eyes); with preproliferative (PPDR) - 13 patients (26 eyes); with
proliferative (PDR) - 25 patients (50 eyes). Used ophthalmic research methods; Laboratory
methods: standard screening methods, special methods of investigation of the
hemostatic system.
Results and conclusions: àctivation of some components of the
hemostatic system in patients with diabetic macular edema (DME) indicates
thrombogenic situation in the microvasculature. Growth parameters: vWf, VIIIf,
protein C SFMK correlates with an increase in the incidence of DME (R1, R2:
0,93; R3 - 0,84; R4 - 0,96), DR and clinical progression of the pathological
process. High cystic diabetic macular edema was detected in 54% of patients
with PPDR and PDR. The combination of genes polymorphism hemostasis in patients
with type 2 gives a synergistic effect on the risk of high cystic macular edema
through increased endothelial activation and dysfunction coagulation and
platelet hemostasis and fibrinolysis inhibition in the retinal
microvasculature. The results obtained can be used in laboratory and clinical
monitoring of hemostasis in patients with DR for the timely diagnosis and
adequate conservative pathogenetic therapy.
Keywords: diabetic macular edema,
endothelial dysfunction, hereditary thrombophilia, hemostasis, diabetic
retinopathy.
Introduction.
Among
the causes of blindness, diabetic retinopathy (DR) is one of the first places.
In patients with type 2 diabetes mellitus (DM 2) DR leads to 10% of low vision
and blindness - 2% of patients [1]. An important component of the pathogenesis
of progression of DR is an imbalance in the hemostatic system and endothelial
dysfunction. Special contribution to the pathogenesis of diabetic complications
make specific microvascular lesions leading to visual impairment. Morphological
and functional changes in the vascular wall in diabetes caused a cascade of
multiple breaches of cell and tissue metabolism caused by prolonged blood
glucose. The accumulation of metabolic pathways of glucose, sorbitol and
fructose leads to increase intracellular osmotic pressure, edema, endothelial
disruption glyco- and phospholipids of cell membranes. Retinal capillary
endothelium, unlike capillary uveal tract, has no pores, and its permeability
is much smaller. Retinal capillary walls are structures gematoretinalnogo
barrier provides the selectivity (selectivity) permeability of various
substances in the transcapillary exchange between the blood and the retina.
Endothelial cells are involved in the regulation of blood clotting components
such as thrombin and fibrin; and angiogenesis, the formation of new blood
vessels. Endothelial dysfunction - is inadequate reduction or increase in the
formation therein of various biological substances [2].
Role of endothelial dysfunction in
the progression of diabetic macular edema (DME) in patients with type 2
sufferers of hereditary thrombophilia, poorly understood [7].
As markers of
endothelial dysfunction is considered: von Willebrand factor (vWf) - adhesive
glycoprotein synthesized by the endothelium of blood vessels. This factor is
synthesized primarily by endothelial cells and elevated levels reflects the
activation or damage to endothelial cells [3].
In plasma vWf forms a complex with
factor VIII, whereby the latter is activated and receives protection from
nonspecific proteolysis, resulting in half-life becomes longer. Another
important function of vWf - promoting platelet adhesion. Soluble fibrin monomer
complexes (SFMK), formed during the degradation of molecules of soluble fibrin
by the action of plasmin. This is one of the earliest markers thrombinemia and
hypercoagulation syndrome. Protein C - physiological anticoagulant. Activated
protein C (APC) inactivates Factors Va and VIII clotting in the presence of its
cofactor - protein S, thereby preventing the transfer of prothrombin into
thrombin. Moreover APS stimulates the secretion of tissue plasminogen activator
by endothelial cells and thus stimulates fibrinolysis [4,5,6].
Since type 2 diabetes is a hereditary disease, the study of hereditary thrombophilia markers acquires greater relevance [7].
Purpose. Study of some parameters of hemostasis, endothelial dysfunction, hereditary thrombophilia markers, clinical and morphological parameters of macular edema in patients with DR on the background 2 diabetes, in combination with hereditary thrombophilia.
Materials and
methods. 50 patients (100 eyes) with DR-2 diabetes. Of these, the
nonproliferative diabetic retinopathy (NPDR) - 12 patients (24 eyes); with
preproliferative (PPDR) - 13 patients (26 eyes); with proliferative (PDR) - 25
patients (50 eyes).
Age of the patients was - 45-62 years. Men - 20 pers, Women - 30 persons. Blood glucose levels in the blood
- 8,7 ± 2,4 (mmol / l). Experience 2 diabetes from 1 year to 10 years.
Complications of type 2 diabetes - hypertension and coronary artery disease -
45 people., Macroangiopathy of the lower limbs - 25 pers., Diabetic nephropathy
- 7 pers., Stroke - 2 persons.
Laboratory studies conducted in laboratory hemostasis
Regional Clinical Hospital ¹ 1 Kemerovo. The material for the study was
deoxygenated blood.
Specific methods of research conducted on
thrombophilia automated coagulometer methods using reagent kits «Dade Behring»
and «Siemens»: definition of activity vWf, antithrombin III, APS, factor VIII
in plasma; determination of resistance to the active factor V protein C (RAPS);
quantitative determination of soluble fibrinmonomernyh complexes (SFMK), a firm
"Technology-standard"; and agregatogramma with inducers of
aggregation ADP ristomycin, collagen, epinephrine.
Detection of lupus antigen (EA) was performed using
"dilution" of thromboplastin, kaolin, Russell viper snake venoms, lebetoksa,
ehitoksa, and confirmatory tests with plasma donor and corrective
phospholipids.
Patients in plasma diagnostics performed PCR
trobofilicheskih gene mutations: Leiden mutation of coagulation factor V
(resistance to activated protein C), prothrombin gene mutation G20210A,
mutation of fibrinogen FGB G-455A, mutation of platelet fibrinogen receptor
GPIIIa 1a / 1b, glycoprotein gene mutation 1F (integrin alpha-2) (GP1A) C807T,
a mutation in the gene for methylenetetrahydrofolate reductase (C 677T MTHFR;
MTHFR 1298); metioninsintazreduk-basins (MTRR A66G); methionine synthase (MTR
A2756G), a polymorphism in the gene for type I plasminogen activator (PAI - 675
4G | 5G), a polymorphism in the gene for coagulation factor XII (FXII C46T), A
polymorphism in the gene for coagulation factor XIII subunit (FXIII G163T,
Val34Leu).
In the examination of the patients used the standard
ophthalmic (visometry, tonometry, perimetry, direct ophthalmoscopy) and special
research methods: (fundus examination with Goldman lens with aspherical lens
"+ 78", fundus fluorescein angiography at the fundus camera «Topkon»,
Japan; optical coherence tomography (OCT) on the unit RTVu-100 firms Optovue
(USA) computer perimetry.
Results
and discussion.
Patients with depression in comparison with the
control group, there is the activation of components of the hemostatic system,
witnesses thrombogenic situations in the microvasculature of retinal vessels.
Increasing the level of vWf in patients with NPDR 22.7% in patients with PPDR -
30.4%, in patients with PDR at 41.4%. The activity of protein C - increases in
patients with NPDR at 16.8%, with PPDR - by 28.2%, with 31.3% of the DA. The
biggest changes concern the activity of factor VIII and SFMK. Factor VIII is
increased in patients with NPDR 33.8% with PPDR - 44.4%, with the DA - 64%, and
SFMK NPDR patients increased by 42.6% compared with the control group had at PPDR
164%, with the DA at 180.5% (Illustration 1).
Illustration 1. Some indicators of hemostasis in patients with
DME with type 2 diabetes before treatment.
vWf -
activity of von Willebrand factor,%; F VIII - Activity Factor VIII,%; Protein -
Protein C activity,%; SFMK - mg%.
* - Significant difference with the norm p ≤0.05
** - Significant difference between the groups of patients and NSPR PPDR
p ≤0.05
*** - Significant difference between the groups of patients PPDR and PDR
p ≤0.05
Increasing values of markers thrombogenic activity (vWf, Factor VIII,
MTA SFMK) in stages HLR confirms its progression, describes occlusion of
retinal capillaries, resulting in the emergence of large areas of circulatory
disorders and increased permeability of small blood vessels of the retina.

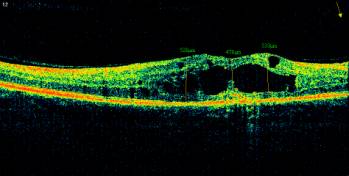
Illustration 2. OCT of the macula and fundus of the right eye of the patient P. 52
years old, diagnosed with PPDR, diffuse cystic macular edema.
Growth indicators
vWf, VIIIf and protein C correlates with an increase in the incidence of
diabetic macular edema in patients with NPDR, PPDR and PDR (R1 -0,93
correlation coefficient vWf with macular retinal thickness in patients with
clinical forms of DR; R2 -0, 93, the correlation coefficient level of factor
VIII with a thickness of the retinal macula in patients with clinical forms
HLR; R3 - 0,84 correlation coefficient of activity of protein C with the
thickness of the macula of the retina in patients with clinical forms HLR; R4
-0,96 SFMK correlation coefficient with a thickness of the retina macular
patients with clinical forms DR).
Illustration 3. The dependence
on the parameters of hemostasis DHS.
vWf - activity of von
Willebrand factor,%; F VIII - Activity Factor VIII,%; Protein - Protein C
activity,%; SFMK - mg%; OCT of the macula - the thickness of the retina, um.
Growth indicators of
endothelial dysfunction (vWf, factor VIII, APS, SFMK) is correlated with an
increase in the incidence of diabetic macular edema and retinal thickness in
the macula in patients with DR. Propotevanie retinal capillaries leads to
retinal edema, diffuse due to leakage of plasma and locally in the formation of
microaneurysms. The first ends with a "soft exudates" and racemose
degeneration, and the second - "hard exudates".
Illustration 4. Types of DHS in patients with
type 2 diabetes.
Patients with non-proliferative DR amid 2 diabetes occurred focal macular edema
in 17% of cases. Against the background of preproliferative DR observed
moderate focal macular edema in 4% of cases, flat diffuse macular edema (18%),
and high diffuse macular edema (4%). When there is a high proliferative DR diffuse
macular edema (43%) and in 7% of cases, a mixed form of diabetic macular edema
(ischemic component with macular traction).
High cystic diabetic
macular edema was detected in 54% of patients with PPDR and PDR. A combination
of several factors, gene mutation: Leiden mutation of the gene V, clotting
factor with MTHFR 1298 - 10% of cases, a polymorphism in the gene ìåòèëåíòåòðàãèäðîôòàëàòðåäóêòàçû (C 677T MTHFR; MTHFR 1298) - 25% of
cases, methionine synthase (MTR A2756G), metioninsintazreduktazy (MTRR A66G) ,
mutation of the glycoprotein 1F (integrin alpha-2) (GP1A) C807T, prothrombin
gene mutation G20210A), polymorphism in the gene I type plasminogen activator
(PAI - 675 4G | 5G), polymorphism in the gene for clotting factor XII (FXII
C46T), a polymorphism in the gene for coagulation factor XIII subunit (FXIII
G163T) - 5% of cases gives a synergistic effect, which is manifested clinically
as high macular edema with cystic vitreoretinal traction in patients with
recurrent retinal venous occlusions with PPDR on background 2 diabetes.
Conclusions: 1. Studies
have shown that growth rates vWf, VIIIf, protein C, SFMK (R1, R2: 0,93; R3 -
0,84; R4 - 0,96) correlates with an increase in the incidence of diabetic
macular edema, the clinical picture DR and progression of the pathological
process.
2. Polymorphism of genes of hemostasis in
patients with type 2 produces the synergistic effect of the high risk of cystic
macular edema through increased endothelial activation and disfuktsii
coagulation and platelet hemostasis and fibrinolysis inhibition in the retinal
microvasculature.
3. The results obtained can be used in laboratory
and clinical monitoring of hemostasis in patients with DR for the timely
diagnosis and adequate conservative pathogenetic therapy.
REFERENCES
1. Ametov A.S., Solovyov O.L. Hemostatic disorders in diabetes and ways
of their correction in combination therapy with metformin and CF Diabeton .//
Sugar diabet.- 2007.- ¹3.- P. 33-39.
2. Santa I.I. , Shestakov M.V., nice little T.M. Diabetes: retinopathy,
nefropatiya.-M., 2001, -176p.
3. Ivanova N.V., Yarosheva N.A. Imbalance in the hemostatic system and
endothelial dysfunction in patients with diabetic retinopathy // Eye magazine.
- 2008.- ¹ 3. - P.33-37.
4. Kretova E.Y. Violations of the hemostatic system in different age
periods in patients with diabetes: Diss. kand.med. nauk.- Tomsk, 2008.-146p.
5. Panteleev M.A. Practical koagulologiya.- M .: Practical Medicine, 2012.-
192p.; yl.
6. Petrishchev N.N., Vlasov T.D. Physiology and pathophysiology of
endothelial // Proc .: Endothelial dysfunction. Causes, mechanisms,
pharmacological korrektsiya. SPb. Univ SPbGMU, 2003.- P.4-38.
7. Severin A.S., Shestakov M.V. Violation of the hemostatic system in
patients with diabetes mellitus // diabet.-2004.-¹1.-P.52-67.
About the Authors:
1. Shelkovnikova Tatyana, Senior Lecturer, Department of Ophthalmology,
MD, a doctor of the laser unit. (t.shelkovnikova@gmail.com, tel. + 7-923-618-19-72)
Kemerovo State Medical Academy of the Ministry of Health of Russia,
Kemerovo
2. Katsadze Junona Leonidovna, Ph.D., Professor, Senior Researcher,
Laboratory coagulation FSI Russian Research Institute of Hematology and Blood
Transfusion, St. Petersburg.
3. Takhchidi Khristo Periklovich, MD, Professor, Vice-Rector of the
medical work, GOU VPO Russian National Research University of N.I. Pirogovà Russian Ministry of Health, Moscow
4. Shishlyannikova Nina Yurievna, Ph.D., assistant professor of biological,
overall, Bioorganic Chemistry and Clinical Laboratory Diagnostics Medical
University KemGMA Health Ministry, Kemerovo.