Shchepilina O.V., Begun
P.I.
Saint Petersburg
Electrotechnical University «LETI»
Dynamic
research of system«thighbone-bone graft-implant» of the rehabilitation
period
The urgency of the rehabilitation problem during
postoperative period after the hip fracture results from the fact that the
thighbone traumatic injury affects the locomotor system kinematic reactions in
general, thus facilitating associated disorders that do not directly result
from the injury, yet worsening the patient’s life.
Despite new implant designs, improved skills of
surgeons, new operation methods implemented, the results stop satisfying
patients as the full recovery period reaches half a year. This is because the
missing is the individual approach depending on the bone tissue condition, the
fracture location. The issue of the bone graft reconstruction at the subcapital
fracture location lacks attention.
However, information technologies development in
medicine, particularly in trauma surgery, orthopedics and biomechanics allows achieving
radically new rehabilitation technology level.
The object of the research is to develop
thighbone diagnostic technique after osteosynthesis with muscle activity and
elasticity module (E, MPa) taken into account at every bone graft remodeling
stage. The algorithm has been developed, the calculations have been carried out
and the analysis and the research have been undertaken for the “thighbone-bone
graft-implant” system stress and stain behavior at various rehabilitation
stages.
The following assumptions were considered while
building the conceptual model:
1) thighbone bone structure is idealized to
comprise two isotropic layers: cortical and spongy;
2) within the thighbone, the fissure is located
at the thighbone neck cross-section and it has uniform isotropic structure,
wherein its mechanical properties change at every osteotylus reconstruction
stage and those are localized within the zone that is free of muscular efforts;
4) dynamic stress is applied to the thighbone
center by axes X, Y, Z (www.orthoload.com).
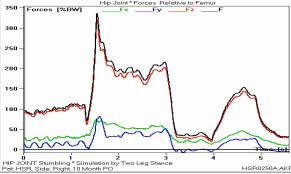
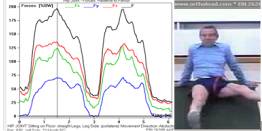
Figure 1 represents experimental data, with the
coordinate system selected (fig.1,a), axes orientation and coordinate center
within the thighbone shown (fig.1,b), as well as the example of the effective
load changes as a function of time (fig.1,c).
|
à |
b |
c |
|
|
|
|
|
Fig.1. Test data |
||
As initial data, the thighbone MRT is used
(fig.2,a) to build the object 3d models (fig.2,b) by means of Mimics, the
computer modeling environment. With those models imported into the Solid Works
software package, a solid thighbone geometric model was obtained with damages
at the area of the greater trochanter (fig.2,c). The considered is the bone
recovery via osteosynthesis, with two cannulated titanium screws (fig.2,d). The
figure2 represents the thighbone MRT slices (a), its 3d model projection with
subcapital fracture, as built via Mimics software (b), and geometric models of
the thighbone neck damage (c) with the thighbone osteosynthesis (d).
|
à |
b |
c |
d |
|
|
|
|
|
|
Fig.2. Benchmark data The graft bone formation process
takes long time (up to 20 weeks). The |
|||
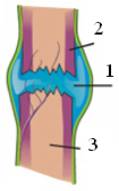
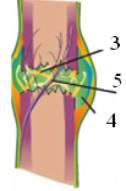
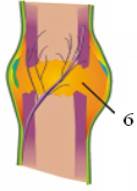
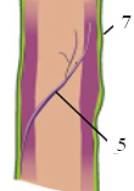
algorithm
considers 4 sequential bone recovery stages (fig.3). The fig.3 contains the
following designations: 1 – hematoma, 2 – cortical layer, 3 – spongy layer, 4 –
cartilage, 5 – blood vessel, 6 – osteotylus, 7 – periosteum, and the
represented are: the inflammation phase (fig.3a), the regenerative phase
(fig.3b-c), and the remodeling one (fig.3d).
|
à |
b |
c |
d |
|
|
|
|
|
|
Fig.3. Schemes inflammatory (A), regenerative (B, C) and
remodeling (D) phases
of callus formation at the femoral neck |
|||
At every stage, the elasticity module is given
according to the diagram of the fig.4 that characterize the graft bone tissue
elasticity module change during the postoperative period.
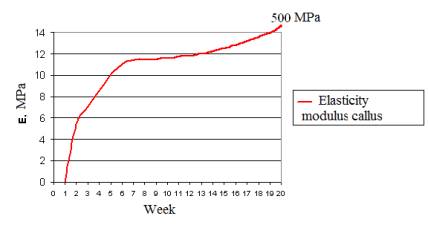
Fig.4. Change elasticity modulus callus
c à
In
terms of non-linear dynamic analysis, various rehabilitation procedures,
relating to the first two rehabilitation stages, were considered. The obtained
results are represented via fig.5,6. The fig.5 represents dependences of
deformations appearing at the first stage with Eper=5.4kPa (a –
experimental data when thigh is move aside, b – experimental data for the thigh
up 30°, c – the results
obtained: 1 – allowed deformation, 2 – deformation with the thigh aside, 3 –
deformation for the thigh up 30°).
|
|
|
|
|
b |
Fig.5.
The first stage of rehabilitation
The fig.5 represents dependences for
deformations appearing at the first stage with Eper=5.4kPa (a –
experimental data when thigh is move aside, b – experimental data for the thigh
up 30°, c – the results
obtained: 1 – allowed deformation, 2 – deformation with the thigh aside, 3 –
deformation for the thigh up 30°).
The fig.6 illustrates three possible ways to
walk at the second rehabilitation stage: walking with support on both legs and
crutches (fig.6a), walking with support on the healthy leg (fig.6b) and walking
with support on the bad leg (fig.6c) with Eper=7.6kPa (1 – support
with both legs, 2 – support with the healthy leg, 3 – support with the bad leg,
4 – the deformation allowed).
Walking
is an important element in the complex process of rehabilitation
and positive effect on the work of many organs: cardiovascular
system, on the pulmonary system improves joint mobility, prevent muscle
degeneration.
The
objectives of the second rehabilitation period are training in the use and development of skills crutches right
away with additional
support from the no-load and
load on the operated leg.
|
à |
b |
c |
d |
|
|
|
|
|
|
Fig.6. Walking on the second
stage of rehabilitation |
|||
The following was concluded there from:
1) the tendency was discovered of the
deformation depending on the elasticity module E, thus this factor must be
taken into consideration when developing rehabilitation programs, particularly
for the initial stages of the rehabilitation, when the bone structure has not
fully restored after the damage yet, and the blood vessels are vulnerable for
significant deformations;
2) putting a thigh aside during the first stage
of rehabilitation, as well as walking with support on the bad leg are
counter-indicative for patients with the subcapital fracture
who underwent osteosynthesis.