A MODIFIED METHOD OF PLASMAPHERESIS IN THE
TREATMENT OF PATIENTS WITH PURULENT CHOLANGITIS
Davlatov S.S.*, Kasymov
Sh.Z.**, Kurbaniyazov Z.B.*, Ismailov A.O.*
*The Chair of Faculty
and Hospital Surgery of Samarkand State Medical Institute’s.
**The Republican
Specialized Center of Surgery named after Academician V.V. Vahidov.
Introduction. The frequency of septic complications of
inflammatory diseases of the biliary tract, despite the attention of
researchers to this issue remains highly relevant. It is believed that without
surgery acute suppurative cholangitis leads to death in 100% of cases (4,6). In
the surgical treatment of cholangitis, significant progress related to the
implementation of modern minimally invasive procedures, but there are a number
of unresolved issues. One of them is holemic endotoxicosis accompanied by
increases in plasma levels of metabolites (bilirubin, urea, creatinine,
residual nitrogen, enzimesoligopeptides of average molecular weight, etc.) (2,5).
Postoperative mortality varies widely, ranging from 8 to 27% (1,3,4). Based on
the fact that the main cause of mortality is endotoxemia, the question
naturally arises of detoxification. Plasmapheresis, is the most extensively
studied by adjuvant therapy. With convincing evidence of effectiveness of
plasmapheresis in purulent cholangitis further research to improve its
efficiency by reducing the amount and possible reinfusion patients treated
purified plasma.
The aim of the study. Improvement of treatment
results biliary sepsis and severe biliary sepsis using an improved method of
plasmapheresis.
Materials and methods. The study was conducted
in the clinic Samarkand medical institute. The basis of the study were 217
patients with hyperbilirubinemia, acute cholangitis, biliary sepsis and severe
sepsis benign biliary origin, complicated by suppurative cholangitis. Most of
the patients were women 136, men were 81. The mean age was 65,3 ± 8,7 years.
In this paper, for the diagnosis of
acute cholangitis and biliary sepsis, we defined the basic laboratory findings
possible to calculate the degree of organ failure on the scale of SOFA (Sepsis
organ failure assessment) and the severity of the systemic inflammatory
response criteria for SIRS (Systemic inflammatory response syndrome).
Laboratory and Diagnostics in addition to accepted clinical blood and urine
tests included the following methods. On the function of the liver was assessed
by bilirubin and its fractions in the blood serum, the activity of serum
transaminases, alkaline phosphatase, protein content and its fractions,
cholesterol levels, prothrombin, indicators thymol and sublimate samples as
well as on the content of electrolytes in the blood serum. Noninvasive
preoperative diagnosis of acute cholangitis, biliary sepsis and pathology gepatopankreatoduodenal
zone, against which they were spent, in addition to physical examination,
including a review of X-rays of the abdomen, ultrasound, computed tomography.
Endoscopic studies included holedohoskopi, fibrogastroduodenoscopy,
laparoscopy, retrograde cholangiopancreatography.
The distribution of patients
according to the etiological basis is presented in Picture. 1.
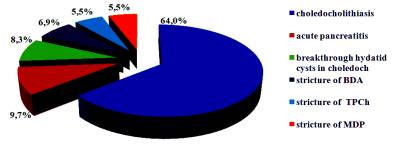
Picture. 1. Distribution of the patients because of obstructive
jaundice.
As seen in the chart, the most
common cause of cholangitis and biliary sepsis is choledocholithiasis 64%,
followed by acute pancreatitis is 9.7%, the third place is a breakthrough
hydatid cysts in choledoch 8.3%, the fourth and fifth accounted for stricture
of the terminal and stricture of the major duodenal papilla, respectively 5.5%
and 5.5%.
The results of the study. All patients were
divided into four groups.
Group 1 - patients with obstructive
jaundice without evidence of an inflammatory response (SIRS = 0) - 85 patients.
Group 2 - patients with obstructive
jaundice and slightly pronounced inflammatory response (SIRS one
characteristic) (acute cholangitis) - 79 patients.
Group 3 - patients with two or more
signs of SIRS (biliary sepsis) - 40 patients.
Group 4 - patients with two or more
signs of SIRS and organ dysfunction SOFA> 0 (severe biliary sepsis) - 13
patients.
In 53 patients with biliary sepsis
and severe biliary sepsis used plasmapheresis, after preliminary minimally
invasive decompression of the biliary tract. After the improvement of the
patients and normalization of peripheral blood counts made
surgery. Of these, 27 patients with a combination of indirect
electrochemical detoxication plasma sodium hypochlorite at 26 with additional
plasma ozonation and subsequent reinfusion detoxify plasma. Types and
characteristics of different methods of plasma exchange are presented in table 1.
Table 1.
Performance indicators indirect combined digitally plasmapheresis.
|
Figures |
IEDP additional ozonation |
IEDP |
|
Reduction of urea |
78,1% |
75,4% |
|
Decrease in
creatinine |
69,9% |
67,6% |
|
Reduction Total bilirubin: Direct Indirect |
90,4% 93,8% 86,9% |
85,4% 92,6% 78,2% |
|
Decrease in total protein |
2,8% |
4% |
|
Reduced albumin |
3,0% |
3,2% |
|
Increase in the
transport function of albumin |
132 |
123 |
|
Decreased concentration (AMWO) |
45,1% |
43,9% |
|
Reduction (LII) |
63,9% |
60,2% |
|
Processing time |
2-3 h |
4-16 h |
The number of sessions of
plasmapheresis ranged from 1 to 3 (of 103 sessions). Rejection of plasma reinfusion
due to lack of detoxification was in 3 cases (methodological and laboratory
error). Otherwise reinfusion
provided 85-90% of circulating plasma total replenishment autoprotein
components in small volumes (600-800 ml) of plasmapheresis. Additionally with was poured fresh
frozen plasma (1doza from one donor) and albumin 10% 100-150 ml, and the
solution Infukoll 6% - 500.0 and crystalloids. Complications during the sessions of
plasmapheresis were observed in 7 cases and were cropped adequate therapy. Contraindications for transfusion to
adequately detoxify autoplasma unknown.
Detoxify plasma before
transfusion were taken out of the container 10 ml plasma biochemical studies. Make sure it is sufficient detoksikated,
the question of the possibility of reinfusion autoplasma as plasma-protection
during a subsequent session programmed plasmapheresis.
Conclusions. Thus,
extracorporeal IEDP and our proposed method is highly effective
preoperative preparation of patients with severe holemic endotoxemia against
jaundice, helps stabilize the activity of cytolytic and cholestatic process,
improves the protein-synthetic function of the liver, as well as allowing to
eliminate the major clinical manifestations in this heavy contingent of
patients, thus greatly expand the indications for surgical treatment.
Additional ozonation eksfuzed
of
plasma after adding to it a solution of sodium hypochlorite can increase
detoxicant effect, reduce the toxicity of the plasma and red blood cells and
prevent the side effects of sodium hypochlorite. Ozone has a biological,
metabolic activity with respect to organic substrates - proteins, lipids,
carbohydrates, shows them the high rate constants. In addition, the additional
impact of ozone can reduce the exposure to 4-16 (with an average of 8-12 hours)
up to 3-4 hours. In general, the method is cheap and effective,
can detoxify the plasma of patients, to minimize the need for donor protein
preparations, reduce the risk of possible immune reactions, the risk of patient
infection hepatitis B and C, human immunodeficiency virus, cytomegalovirus,
herpes.
Literature
1. Akhaladze
G.G.
and other. Clinical stage of suppurative cholangitis. // Annals of Surgical
Hepatology -1997. - ¹ 2. – P. 103-109.
2.
Halperin E.I. Akhaladze
G.G. Biliary sepsis: some features of the pathogenesis // Surgery. - 1999. - ¹
10. - P. 16-19.
3.
Davlatov
S.S., Kasymov Sh.Z., Kurbaniyazov Z.B., Rakhmanov K.E., Ismailov A.O.
Plasmopheresis in the treatment of cholemic endotoxicosis // Academic Journal
of West Siberia ¹ 1, 2013. P.
30-31.
4. Syusyukin
A.E. Kostyuchenko A.L. Belsky A.N. etc. Modern efferent therapy in clinical
toxicology // Efferent therapy-2004. ¹ 3.-P. 69-71.
5.
Shapovalyants S.G. and
other endoscopic techniques in the treatment of post-surgical scar stricture of
bile ducts. // Annals of surgical hepatology -2007. - ¹ 2. – P. 70-77.
6. Kondrup
J., Almdal T., Vilstrup High H. volume plasma exchange in fulminant hepatic
failure (et
al.)
Int. J. Artif. Organs. - 1992. - N 15. - P. 669 - 676.